LAPAROSCOPIC GYNAECOLOGIST
Laparoscopic Gynaecologist in Ahmedabad
Gynaecologic Laparoscopy is a hybrid surgical approach that has become a popular alternative to open surgery. While open surgery usually requires a larger incision, laparoscopy involves the use of a laparoscope to examine your pelvic or abdominal area.
If you are experiencing pelvic pain, have a history of pelvic infection or are facing infertility issues, then laparoscopy may be the way to go.
Benefits of Laparoscopy over Laparotomy
As compared to an Open abdominal surgery or a Laparotomy, Laparoscopy is considered a better alternative as it involves smaller incisions. In addition, it causes lesser postoperative pain, leaves fewer scars and needs a shorter convalescent period for recovery.
Gynaecologic Laparoscopy can be applied for diagnosis, treatment or a combination of the two. There are a variety of diagnosis and treatment applications that the best laparoscopic gynaecologist in Ahmedabad, Gujarat use today.
Applications of Laparoscopy: Diagnosis
Using a laparascope to study your abdominal or pelvic area, your laparoscopic gynaecologist can identify and diagnose conditions such as endometriosis, pelvic inflammatory disease or reproductive cancers. They can find evidence of infertility or ectopic pregnancy, or come across uterine fibroids, pelvic abscesses (pus) or pelvic adhesions (scar tissue)
Applications of Laparoscopy: Treatment
Laparoscopy can also be used for treatment, through surgeries such as tubal ligation or surgical. In fact, tubal ligation was the main application of laparoscopy procedures about 25 years back. Today, its applications extend to hysterectomy or removal of the uterus, removal of the ovaries, removal of ovarian cysts and the removal of fibroids as well. It can reverse tubal ligation as well, help block blood flow to fibroids and treat endometriosis through endometrial tissue ablation. A prolapsed uterus can be treated through vault suspension, while incontinence is treated by using the Burch procedure.
What you need to know about the procedure
Prior to a laparoscopy diagnosis, your doctor may assess the condition of your abdominal wall and peritoneal cavity to determine your readiness for the procedure. They could also ask you to carry out routine bloodwork or imaging tests, and fast prior to the procedure.
The procedure is carried out under general anaesthesia, and your laparoscopic gynaecologist will use a laparoscopic camera to study your lower abdomen. They will be able to examine your uterus, fallopian tubes, ovaries, bladder and bowel. A biopsy may be carried out if required - that is, a small sample of tissue may be extracted during the laparoscopy for further diagnosis.
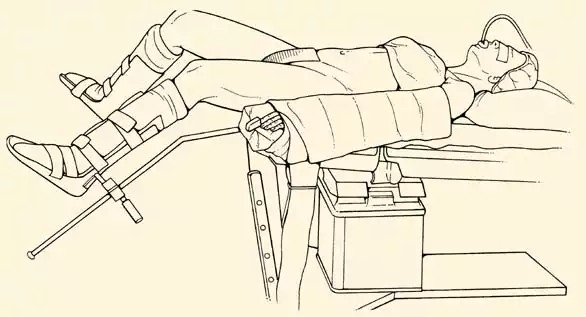
Low lithotomy position with legs in stirrups
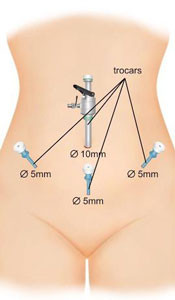
Insertion of ports
After a laparoscopic surgery: Postoperative course
Laparoscopic surgeries are usually carried out quite smoothly. It may take 24 hours for the anaesthetic to wear off, and you can begin gradual oral feeding from the next day itself. Discharge can take between 1 to 3 days, and any mild abdominal wall pain that you experience can be treated with medication.
Rarely, there could be complications such as severe pain, nausea or vomiting, which should subside soon. In case you are facing serious complications, such as prolonged nausea, fever over 101 degrees Fahrenheit, bleeding or pus production, urinary problems, thromboembolism or any injury to your blood vessels or pelvic organs, please contact your doctor immediately. Please note, if you are suffering from extreme endometriosis, have had abdominal surgery in the past, or are extremely underweight or overweight, the likelihood of complications increases.
HYSTEROSCOPY
Hysteroscopy is a minimally invasive surgical procedure used to evaluate or treat conditions such as abnormal uterine bleeding, severe and heavy menstrual periods, scarring and uterine growths such as fibroids or polyps. It can also be used to examine potential malignancy in post-menopausal patients.
It can be used to diagnose and treat causes of abnormal bleeding and involves inspection of the uterine cavity through endoscopy. Diagnostic hysteroscopy involves the diagnosis of intrauterine pathology while while operative hysteroscopy serves as treatment or a method for surgical intervention.
How is hysteroscopy performed?
When a hysteroscopy is carried out for diagnostic purposes, it can be performed with just local or regional anesthesia and can take between 5 minutes to 30 minutes. A salt or sugar solution is used to distend the uterus, and a small-diameter camera is inserted into the vagina to examine the cervix and the uterus. Operative hysteroscopy can take longer and may need general anesthesia. In many cases, both diagnosis and treatment are carried out during the same procedure. Hysteroscopy is carried out on an outpatient basis.
What are the benefits of hysteroscopy?
A hysteroscopy is a relatively quick procedure with a fast recovery time. Most patients are discharged on the same day. Since no abdominal wound is created for this procedure, there is minimal postoperative pain.
Should you consider an endometrial ablation instead?
An endometrial ablation may be a good alternative to hysteroscopy for mothers with extreme or heavy bleeding, where fibroids or any intrauterine pathology have been ruled out as a cause. This is an outpatient procedure, and can significantly reduce bleeding. Make note that pap tests and pelvic exams are still required regularly after an endometrial ablation, and that patients with endometrial cancer, precancer, severe dysmenorrhea (menstrual cramps) or a uterine cavity larger than 12 centimetres should avoid this procedure.
After a hysteroscopy: Recovery
The absence of incisions leads to a quick recovery time after a hysteroscopy. Mild pain medication after the surgery, such as a simple anti-inflammatory medicine, usually suffices in dealing with postoperative discomfort. Patients should avoid sexual intercourse, sports, intensive activities and insertion of objects such as a tampon in the vagina for two weeks after the surgery. Women can return to work after a two-week period of rest and recovery as well.
Precautions
While this is a fairly safe procedure, on some occasions the uterus or cervix can be punctured. A good and experienced surgeon will avoid this, although you may experience some discomfort, similar to period pain, after the surgery. Nausea or lightheadedness and mild bleeding is common. However, if you experience severe pain, excessive bleeding or vaginal discharge, an inability to urinate or have a fever over 100 degrees Fahrenheit,
Do you have any questions? or if you’d like to book a confidential appointment.
